Information for Persons Who Are Immunocompromised Regarding Prevention and Treatment of SARS-CoV-2 Infection in the Context of Currently Circulating Omicron Sublineages — United States, January 2023
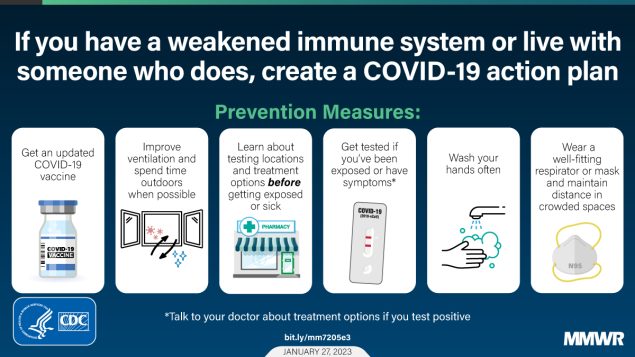 live with someone who does can take. The title states, “If you have a weakened immune system or live with someone who does, create a COVID-19 action plan.” The graphic includes six boxes that describes prevention measures, “Get an updated COVID-19 vaccine. Improve ventilation and spend time outdoors. Learn about testing locations and treatment options before getting exposed or sick. Get tested if you’ve been exposed or have symptoms. Wash your hands often. Wear a well-fitting respirator or mask and maintain distance in crowded spaces.”" />
live with someone who does can take. The title states, “If you have a weakened immune system or live with someone who does, create a COVID-19 action plan.” The graphic includes six boxes that describes prevention measures, “Get an updated COVID-19 vaccine. Improve ventilation and spend time outdoors. Learn about testing locations and treatment options before getting exposed or sick. Get tested if you’ve been exposed or have symptoms. Wash your hands often. Wear a well-fitting respirator or mask and maintain distance in crowded spaces.”" />
As of January 20, 2023, >90% of circulating SARS-CoV-2 variants in the United States, specifically Omicron BQ.1, BQ.1.1, XBB, and XBB.1.5 sublineages, are unlikely to be susceptible to the combined monoclonal antibodies, tixagevimab and cilgavimab (Evusheld) used for preexposure prophylaxis against SARS-CoV-2 infection (1). The Food and Drug Administration announced on January 26, 2023, that Evusheld is not currently authorized for preexposure prophylaxis against SARS-CoV-2 infection in the United States (2). It is important that persons who are moderately to severely immunocompromised,* those who might have an inadequate immune response to COVID-19 vaccination, and those with contraindications to receipt of COVID-19 vaccines, exercise caution and recognize the need for additional preventive measures ( Box). In addition, persons should have a care plan that includes prompt testing at the onset of COVID-19 symptoms and rapid access to antivirals if SARS-CoV-2 infection is detected.
COVID-19 vaccination remains the most effective way to prevent SARS-CoV-2–associated serious illness, hospitalization, and death. All persons, including those who are immunocompromised and their household members and close contacts, should stay up to date with COVID-19 vaccination, and receive the updated (bivalent) booster dose, when eligible. † Although persons who are moderately to severely immunocompromised might not mount a strong vaccine-mediated immune response, staying up to date with COVID-19 vaccination § does provide some protection (3,4). A recent CDC study of preliminary data showed that a bivalent booster dose provided additional protection against symptomatic SARS-CoV-2 infection among immunocompetent persons who had previously received 2, 3, or 4 monovalent vaccine doses (4).
Despite evidence of vaccine effectiveness, coverage with the bivalent booster dose across the United States remains low. As of January 18, 2023, 15.3% of persons aged ≥5 years had received a bivalent booster dose (5). CDC recommends that all eligible persons aged ≥6 months receive 1 bivalent booster dose. Persons are eligible for a bivalent booster dose if they are aged 6 months–5 years and have completed a Moderna COVID-19 primary series ≥2 months earlier. Persons aged 6 months–4 years and who received a 2-dose Pfizer COVID-19 primary series ≥8 weeks earlier can receive the bivalent booster as their third dose.
Among persons with immunocompromise and their household members and close contacts, prevention measures ¶ including wearing a high-quality and well-fitting mask,** maintaining physical distance from others (≥6 ft [1.8 m]), improving indoor ventilation, †† practicing frequent handwashing, and developing a care plan, §§ should be considered in addition to receipt of a bivalent booster dose. It is important to wear a mask and maintain physical distance from others if it is not possible to avoid crowded indoor spaces. In addition, simple interventions should be used to improve ventilation in buildings and decrease SARS-CoV-2 transmission by improving air flow. CDC has developed interactive tools ¶¶ to help identify ways to improve ventilation in the home. In-duct ultraviolet germicidal irradiation lights can also be added to home heating ventilation and air conditioning systems to inactivate SARS-CoV-2 as air passes through the system.*** Frequent handwashing with soap and water is the best way to eliminate germs in most situations. If soap and water are not readily available, an alcohol-based hand sanitizer containing ≥60% alcohol is a good alternative. Also, it is important for persons who are immunocompromised to develop a care plan in consultation with their physician, in the event that they develop COVID-19.
Persons with mild to moderate symptoms of COVID-19 who 1) are aged ≥50 years, 2) have an underlying health condition ††† (especially moderate to severe immunosuppression), or 3) are unvaccinated are at risk for severe COVID-19–associated outcomes. Irrespective of vaccination status, symptomatic persons who are immunocompromised, their household members, and their close contacts should be tested for SARS-CoV-2 infection as soon as possible and receive treatment within 5–7 days of symptom onset. Early outpatient treatment of mild to moderate COVID-19 with a recommended first-line therapy, ritonavir-boosted nirmatrelvir (Paxlovid) or remdesivir (Veklury), or the second-line therapy, molnupiravir (Lagevrio), have been shown to reduce the risk for severe COVID-19, including hospitalization and death. §§§ These medications are expected to retain activity against the currently circulating Omicron sublineages (6) and are widely available. ¶¶¶ Available COVID-19 treatment does not supplant the need for persons to stay up to date on their COVID-19 vaccinations, which are highly effective at preventing COVID-19–related morbidity and mortality.
Corresponding author: Pragna Patel, plp3@cdc.gov.

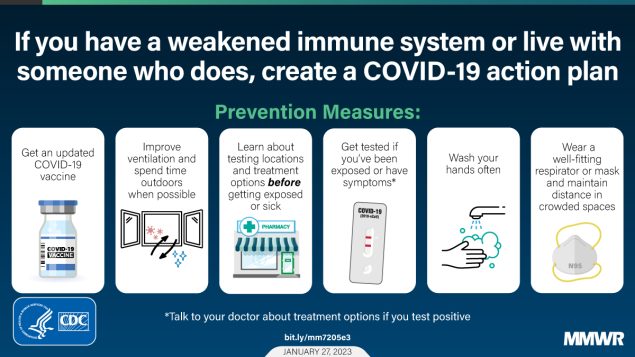 live with someone who does can take. The title states, “If you have a weakened immune system or live with someone who does, create a COVID-19 action plan.” The graphic includes six boxes that describes prevention measures, “Get an updated COVID-19 vaccine. Improve ventilation and spend time outdoors. Learn about testing locations and treatment options before getting exposed or sick. Get tested if you’ve been exposed or have symptoms. Wash your hands often. Wear a well-fitting respirator or mask and maintain distance in crowded spaces.”" />
live with someone who does can take. The title states, “If you have a weakened immune system or live with someone who does, create a COVID-19 action plan.” The graphic includes six boxes that describes prevention measures, “Get an updated COVID-19 vaccine. Improve ventilation and spend time outdoors. Learn about testing locations and treatment options before getting exposed or sick. Get tested if you’ve been exposed or have symptoms. Wash your hands often. Wear a well-fitting respirator or mask and maintain distance in crowded spaces.”" />