

Please encourage interested patients to view our Medicare Advantage plans.
The Sample ID Cards section of the EmblemHealth Provider Manual shows representative ID cards for all our members.
The ID cards show when a referral is needed for a specialist visit. Plans that do not need a referral state “No Referral Required” on the ID card.
Here is a sample of our standard ID card:
When a ConnectiCare logo appears on an EmblemHealth Medicare ID card, it means ConnectiCare Choice Network providers can see the member.
Please note VIP Dual members enrolled in the Integrated Benefits for Dual Eligible (IB Duals) plans in 2023 will be disenrolled at the end of the year and will need to select a new Part D plan to keep their prescription drug coverage. Affected members will receive a non-renewal letter with instructions on how to select a new plan.
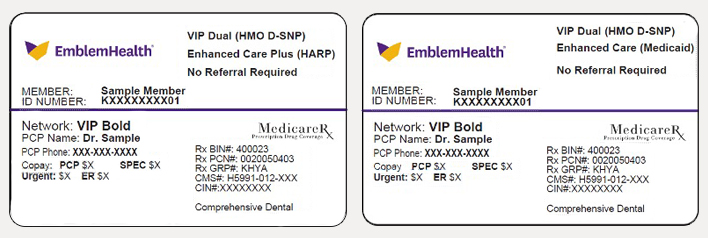
Here are sample ID cards for the IB Dual plans being reintroduced in 2024 under the new plan contract ID.
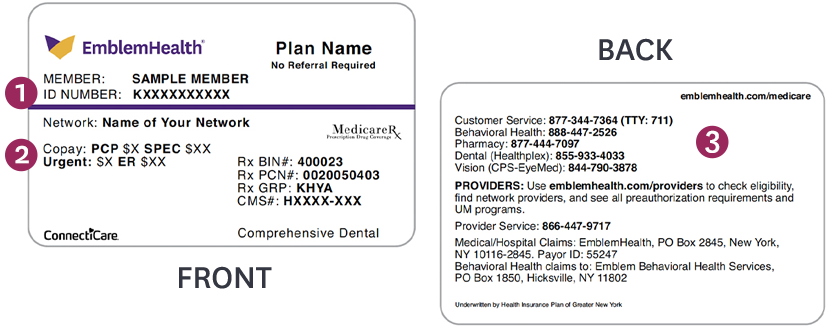
 | Member ID number. |
 | Copays for PCPs, specialists, urgent care, and emergency care. |
 | List of important phone numbers. |
Please refer to your ID card to see if it has the ConnectiCare logo. This means you can use providers in Connecticut.
If you have a dental benefit, you will have contact information for Healthplex on the back of your ID card. Healthplex has been selected to administer dental benefits to you in 2022. Please note that your primary care provider’s (PCP) name is no longer printed on your ID card. You can find the name of your PCP or select a new PCP by signing in our member portal.
For plan details and complete lists of the Medicare plans offered, see:
Integrated Benefits for Dual Eligible (IB-Duals) Program.
In 2023, some of our members were retroactively enrolled into the Integrated Benefits for Dual Eligible (IB-Duals) Program. This triggered the need to recoup payments made under the members’ old plans and reprocess the claims under their new one. See full explanation in the article IB-Dual Program – Claims Reprocessing Under New Member IDs.
We are making some changes to the IB-Duals Programs offered in 2024. IB-Dual members who have the EmblemHealth VIP Dual (HMO D-SNP) plan will be disenrolled as of Dec. 31, 2023, as we will no longer be offering this plan. Affected members will receive a non-renewal letter with instructions on how to select a new Part D plan to keep their prescription drug coverage.
Some of our Medicare plans allow members to see providers in both EmblemHealth and ConnectiCare plans. The summaries of companies, lines of business, networks, and benefit plans above indicate whether there is reciprocity between the companies, and which networks the members may use. When a ConnectiCare logo appears on an EmblemHealth Medicare member ID card or an EmblemHealth logo is on a ConnectiCare Medicare member ID card, it means reciprocity is in place and the affiliate language in the provider agreements apply. This allows the member to see providers in both companies’ Medicare networks. The member’s underwriting company will determine the policies and procedures that must be followed.
To easily determine if you or a provider you manage is in-network for an EmblemHealth or ConnectiCare member, use the Check Provider Network Status look-up tool in the Member Management section of the provider portal. Our provider portals are connected, so you may conduct business for both EmblemHealth and ConnectiCare members in one place.
All VIP Medicare plan members need to select a primary care provider (PCP). If a member fails to select a PCP, EmblemHealth will assign one. For certain members, the selected or assigned PCP can be found on the member’s ID card. You can also locate the assigned PCP on the Member Details page when you check the member’s eligibility in the provider portal. Providers can see their assigned plan of members by running a PCP Member Panel report using our provider portal.
EmblemHealth is modifying its Medicare plan portfolio. The following plans will not be offered in 2024:
For helpful resources to assist your practice in coordinating care for EmblemHealth members, see Clinical Corner and the Utilization and Care Management chapter of the EmblemHealth Provider Manual. For ConnectiCare members, see Clinical Information and Coverage Guidelines.
Medicare special needs plan members will receive a call from EmblemHealth asking them to complete the health assessment (HA). Please encourage your members to complete this survey. This will help our Care Management team direct them to appropriate care and support services. Members may also be eligible for EmblemHealth’s Member Rewards Program when completing their HA within the first 90 days of enrollment, and annually thereafter.
In 2024, EmblemHealth will continue to offer Medicare Advantage and special needs plan members the EmblemHealth Member Rewards Program to encourage them to receive primary care and key health screenings. Members may be eligible to receive a reloadable reward card with $10 to $100 for each of the eligible services they complete. Please reach out to your patients to schedule these important preventive exams. Members can see a list of possible rewards and earned rewards by signing in to the member portal and following prompts for Wellness Rewards. Once they register for the rewards, they will be able to receive their reward card as they complete reward activities.
Claims must be received by Dec. 31 of the calendar year for the incentive to be paid. Members must receive and redeem the reward before Dec. 31, 2024. Only one reward can be earned for each health service shown in the table below.
| Activity | Eligible Medicare Population | Reward Trigger/ Description | Incentive Frequency | Incentive Per Activity |
|---|---|---|---|---|
| EmblemHealth Member Portal Registration | All members not yet registered | Create a new EmblemHealth Member portal account in the calendar year. | Once a lifetime | $25 |
| Sign up for paperless materials | All members | Complete process to sign up for paperless materials. | Once a lifetime | $25 |
| Initial Health Assessment (90 days) | All new members | Complete assessment within 90 days of enrollment | Once a year | $50 |
| Annual Health Assessment | D-SNP members only | Complete assessment within calendar year (by D-SNP member). | Once a year | $50 |
| Initial Medicare Annual Well-Visit (90 days) | All new members | Complete a Medicare annual well-visit within 90 days of Medicare eligibility. | Once a year | $50 |
| Colorectal Cancer Screening | Members, ages 40+ | Complete a fecal occult blood test (FOBT), flexible sigmoidoscopy, colonoscopy, FIT DNA test, or colonography. | Once a year | $25 |
| Diabetes A1C Test | Diabetic members, ages 18+ | Complete an A1C blood test. | Once a year | $25 |
| Diabetes Eye Exam | Diabetic members, ages 18+ | Complete a retinal or dilated eye exam by an eye care professional. | Once a year | $25 |
| Mammogram Exam | Women, ages 40+ | Complete a mammogram. | Once every two years | $50 |
| Kidney Health Evaluation | Diabetic members, ages 18+ | Complete an estimated glomerular filtration rate (eGFR) test and a urine albumin-creative ratio within the calendar year | Once a year | $25 |
| Bone Mineral Density (BMD) Test | Women with a fracture | Complete a BMD within six months after fracture | Once a year | $100 |
In addition, VIP Dual and VIP Dual Reserve DSNP members who are eligible to participate in our Medication Therapy Management Program and complete a comprehensive medication review with one of our pharmacists can earn rewards for filling Select Care Drugs (Tier 6) medications for high blood pressure, high cholesterol, and diabetes. Annual PCP visit reward is not offered in 2024.
Enrollees covered under our dual-eligible special needs plans (D-SNPs) have care plans on file with our Care Management team. We make care plans available to providers on our provider portal unless they contain sensitive information.
If you do not see an expected care plan posted on the portal, contact us to receive a copy.
EmblemHealth:
Phone: 800-447-0768, Monday through Friday, 9 a.m. to 5 p.m.
ConnectiCare:
Phone: 800-390-3522, Monday, Thursday, and Friday, 8 a.m. to 4 p.m., or Tuesday and Wednesday, 8 a.m. to 7:30 p.m.
Our Medicare members will have continued access to Medicare Connect Concierge in 2024. This is the one phone number members can call when they need help solving their health care needs. Medicare Connect Concierge can help:
To reach Medicare Connect Concierge, please call 877-344-7364 (TTY: 711), 8 a.m. to 8 p.m., seven days a week.
If you provide clinic visits to our Medicare members and are owned and operated by a hospital, please review our clinic visit policy and correct coding requirements.
Reminder: For services rendered in place of service (POS) 19, off-campus hospital-owned location, claims billed with the G0463 clinic code should include the Modifier PO.
For helpful claims resources for EmblemHealth members, see Claims Corner and the Claims chapter of the EmblemHealth Provider Manual; for ConnectiCare members, see Billing and Claims and Our Policies.
Contracted time frames in provider agreements will supersede time frames in this guide. For facility time frames, see the EmblemHealth Provider Manual or applicable agreement.
ConnectiCare offers two plans to members who have Medicaid (Choice Dual and Choice Dual Vista). In addition, many Qualified Medicare Beneficiaries (QMBs) enroll in our Medicare Advantage plans. Members with full Medicaid or QMBs are not responsible for paying any member cost-share for their plan-covered benefits.
Medicare-Medicaid full dual eligible and QMB individuals who qualify to have their Medicare Parts A and B cost-share covered by their state Medicaid are not responsible for paying their Medicare Advantage plan cost-shares for Medicare-covered Part A and Part B services. Please do not balance bill these members.
Federal and New York state laws prohibit providers from balance billing Medicare-Medicaid dual eligible individuals for any Medicare deductibles, coinsurance, or copayments. All Medicare and Medicaid payments, if any, received for services provided to dual eligible individuals must be accepted as payment in full. To comply with this requirement, providers treating dual eligible and QMB individuals enrolled in an EmblemHealth Medicare Advantage plan must do the following:
Federal law and provider contracts prohibit Medicare (EmblemHealth)-enrolled providers from balance billing beneficiaries with Medicare and QMB, and Medicaid providers from balance billing dual eligibles. Providers may reference Section 1902(n)(3)(B) of the Social Security Act, as modified by Section 4714 of the Balanced Budget Act of 1997.
For EmblemHealth members, you can use eMedNY to check whether the member has full or partial Medicaid benefits. For more detail, call the New York State eMedNY Call Center at 800-343-9000 Pharmacy providers may use this Pharmacy Balance Billing guide for instructions on coordinating benefits with New York State’s eMedNY program.
For ConnectiCare members, you can contact the Connecticut Department of Social Services at 800-842-8440.